Medicare's AI Takeover: When Algorithms Decide Your Healthcare
How Washington Turned Your Medical Decisions Into Silicon Valley Profit Centers
You schedule that knee surgery your doctor recommended. Same Medicare card. Same copay.
Then you discover a computer algorithm, trained by a for-profit tech company that gets paid to deny your care, now decides whether you actually need the procedure.
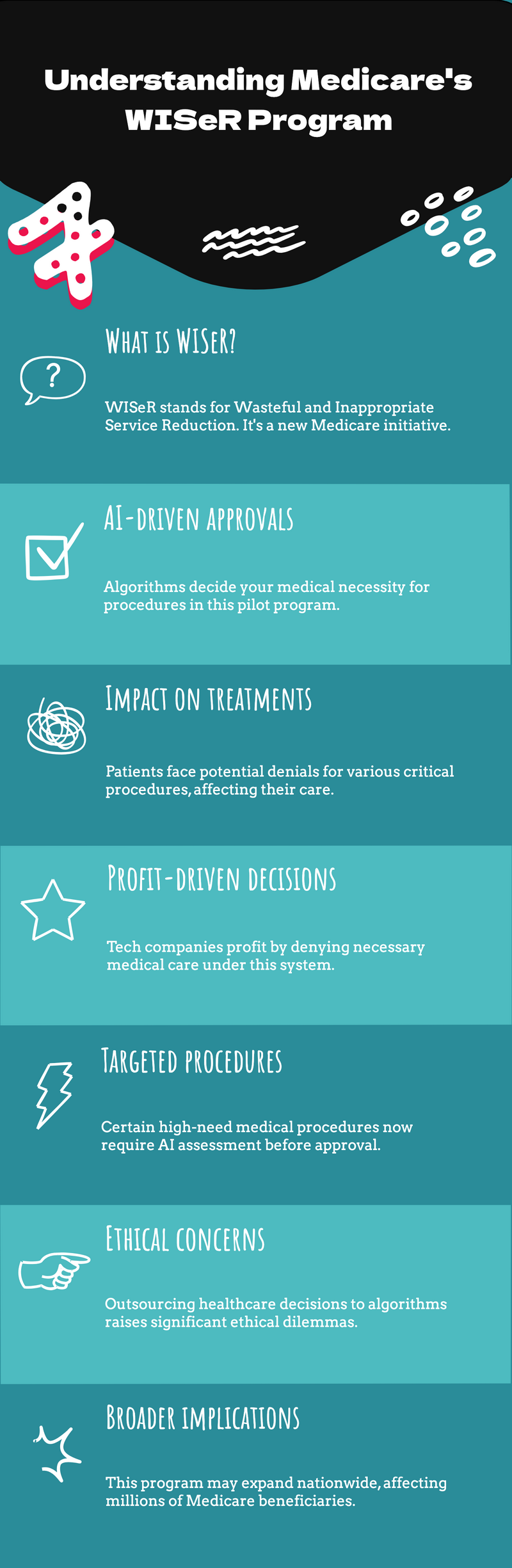
Welcome to WISeR: Washington's latest Medicare "innovation."
This isn't some dystopian future scenario. Starting January 1, 2026, millions of seniors in six states will become test subjects in the most radical transformation of Medicare since its creation.
The "Wasteful and Inappropriate Service Reduction" model — announced quietly on a Friday afternoon in June 2025—represents the largest expansion of AI-driven healthcare rationing in American history.
Silicon Valley Meets Your Surgery
Picture this: You need deep brain stimulation for Parkinson's disease. Your neurologist, who's treated you for years, believes it's medically necessary. But before Medicare pays, your case gets fed into an artificial intelligence system operated by a tech company that profits when they say no.
The algorithm screens your medical records, insurance history, and treatment patterns. Most approvals happen automatically—the easy money. But if the AI flags your case as "questionable," it gets bumped to a human reviewer. Not your doctor. Not an independent medical expert. A clinician employed by the same company that just made money by questioning your care.
This is happening right now in New Jersey, Ohio, Oklahoma, Texas, Arizona, and Washington. Nearly one in five Medicare beneficiaries in those states will face this system for a carefully selected list of medical procedures that CMS claims are "vulnerable to fraud, waste and abuse."
The AI Hit List: What's Really Under Attack
Here's exactly what CMS is targeting—every procedure that will require permission from an AI algorithm before Medicare pays:
Neurological Treatments:
- Deep brain stimulation for Parkinson's disease and essential tremor
- Vagus nerve stimulation for seizures
- Electrical nerve stimulators for chronic pain
- Hypoglossal nerve stimulation for sleep apnea
Pain Management:
- Epidural steroid injections for back pain
- Induced lesions of nerve tracts for chronic pain
Spinal Procedures:
- Cervical fusion surgery
- Percutaneous vertebral augmentation for spinal fractures
- Image-guided lumbar decompression for spinal stenosis
Wound Care:
- Skin and tissue substitutes for chronic wounds
- Bioengineered skin products for diabetic ulcers
- Cellular tissue-based wound treatments
Other Critical Services:
- Arthroscopic knee surgery for osteoarthritis
- Sacral nerve stimulation for incontinence
- Incontinence control devices
- Diagnosis and treatment of impotence
Look at that list. These aren't cosmetic procedures or experimental treatments. They're interventions for Parkinson's disease, chronic pain, diabetic complications, and spinal conditions that devastate quality of life for millions of seniors.
Having spent decades in healthcare leadership, I've seen utilization management evolve. But I've never witnessed anything as cynical as paying Silicon Valley companies a percentage of the healthcare dollars they prevent from being spent on treatments like these.
Well, maybe I have.
The Bounty Hunter Business Model
Here's the part that should terrify every American approaching Medicare age: these technology vendors get paid based on "demonstrated reductions in spending for medically unnecessary services." Translation? The more care they deny, the more money they make.
Sound familiar? It should. This is the exact same "bounty hunter" payment model that created the notorious Recovery Audit Contractors (RACs) – private companies that got rich clawing back Medicare payments after the fact. Except now, instead of recovering money after treatment, these AI systems block treatment before it happens.
CMS is literally creating financial incentives for companies to stand between you and your doctor's medical judgment. The CMS Innovation Center calls this "leveraging private sector innovation." I call it healthcare extortion with a computer science degree.
The most unconscionable part? While the administration was simultaneously announcing voluntary commitments from private insurers to reduce prior authorization barriers, they were building new AI-powered barriers for traditional Medicare beneficiaries.
And let me assure you that private insurers would never get away with this same approach.
The Great Medicare Betrayal
For sixty years, traditional Medicare's core promise was simple: if you need medical care and it's covered, you get it. No insurance company bureaucrat second-guessing your doctor. No prior authorization maze. Just healthcare when you need it.
That promise officially dies on January 1, 2026.
Traditional Medicare beneficiaries chose their coverage specifically to avoid the prior authorization nightmares plaguing Medicare Advantage plans. Now, the CMS Innovation Center has brought the worst aspects of managed care – AI-driven denials, profit-motivated reviews, administrative delays – directly into the heart of original Medicare.
The cruelest irony? CMS claims this will reduce the 25% of healthcare spending they label as "waste." But their own cited research shows only 11% of healthcare waste comes from clinical overuse. The other 89% stems from administrative complexity, pricing failures, and coordination breakdowns.
Their solution to administrative waste? Create more administrative middlemen.
When Machines Override Medicine
The AI systems making these decisions have never examined a patient, never felt the tremor of Parkinson's progression, never witnessed the impact of chronic pain on daily living. They process data points: age, diagnosis codes, utilization patterns, cost projections.
What they can't process: the human context that makes each medical decision unique.
When you look at that list of targeted procedures, you're seeing treatments for some of the most debilitating conditions affecting seniors. Diabetic wound care that prevents amputations. Deep brain stimulation that gives Parkinson's patients their mobility back. Spinal procedures that restore the ability to walk without excruciating pain.
Having navigated healthcare transformations as a CEO, somewhat of an expert in AI, and a physician, I understand the appeal of technology solutions. But medicine isn't a coding problem. It's a human problem requiring human judgment, especially when that judgment involves the most vulnerable patients in our healthcare system.
The Expansion Trap
Here's what makes WISeR particularly dangerous: this six-state pilot is explicitly designed for rapid nationwide expansion. The CMS Innovation Center can roll this out to all fifty states without Congressional approval if the program meets its cost-savings targets.
The program was deliberately structured as a demonstration project under Section 1115A authority, avoiding the legislative oversight that would normally govern such a radical policy shift. The bet is that by the time Americans understand what's happening, the infrastructure for AI-driven healthcare rationing will be too entrenched to dismantle.
Current Medicare beneficiaries outside the six pilot states should pay attention: you're next. The only question is whether the expanding program will target more procedures, more conditions, or simply more states first.
What We're Really Trading Away
CMS estimates this pilot could save $1.9 to $5.8 billion annually by eliminating "low-value" services. But they're not accounting for the human cost of delayed diagnoses, progression of untreated conditions, and the psychological trauma of having algorithms question your medical needs.
When my mother needed cataract surgery at 85, Medicare covered it without question. She got her vision back and still lives independently. She still even has a driver's license. Under an expanded WISeR, that same surgery might require prior authorization from an AI system trained to find reasons to say no.
The current approach trades Medicare's fundamental commitment to beneficiary access for Silicon Valley's promise of algorithmic efficiency. They're treating healthcare like a logistics problem instead of a human right.
The Bottom Line
WISeR represents the most fundamental betrayal of Medicare's founding principles in the program's six-decade history. By outsourcing medical necessity decisions to profit-motivated AI systems, policymakers have transformed America's most trusted healthcare program into a testing ground for algorithmic rationing.
We’re witnessing not progress, but the corporate capture of the medical decision-making process.
The saddest part?
Americans who spent their working lives paying into Medicare, believing it would be there when they needed it, are about to discover their healthcare decisions have been handed over to companies that profit from saying no.
Have you or someone you know faced prior authorization delays for necessary medical care? What's your biggest concern about AI systems making healthcare decisions? Share your thoughts below.
I’m dedicated to exposing parts of the healthcare system that prioritize profits and bureaucracy over genuine patient care and well-being. I welcome your comments, ideas, and feedback for future articles. If you see an aspect of the healthcare system that deserves more attention, please reach out and share your perspective—your input helps drive important conversations forward.
#Medicare #WISeR #HealthcarePolicy #AIinHealthcare #PriorAuthorization #MedicalAI #PatientRights #HealthcareReform

Member discussion